Surviving an Attempt at Suicide
- My Niche Is Human
- Episode 7
- 38 minutes
- Interview
- Depression, Esteem, Family, Mental Health, Relationships, Safety
Show Notes
- The difficulty of putting into words the power of the hopeless feeling that leads us to feel like there are no other options…
- Realizing that acceptance alone does not bring peace, you must work to Heal
- Finding the spark that comes from surviving the dark moments when they return
- Paying attention to the signs
- How you can help your loved ones who may be struggling
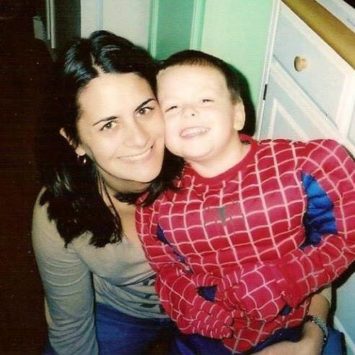
A conversation with my sister, Maggie
Have you ever considered hurting yourself, or do you know someone who has considered, attempted, or completed Suicide? My sister, Maggie, attempted this almost 4 years ago. She was courageous enough to agree to come on the show and share her story hoping to give just one person, hope.
This is not an overly tactical nor a How-to episode, but rather a heart-to-heart conversation between two siblings sitting at the kitchen table. I feel many of us are guilty of always trying to solve problems, myself included. This was a valuable lesson for me to realize that sometimes there is greater power in simply sitting down, and listening.
If you’re currently having trouble talking about your own feelings with yourself, or a loved one, check out the episode before this on How to Talk about Your Mental Health. I hope you can take the time to listen to this episode. – If you feel inspired to reach out or leave a note to Maggie, she is open to and can be contacted through DM on her Instagram
Resources Mentioned
Surviving an Attempt at Suicide
Steven: [00:00:00] This is episode number seven of the, my niche is human podcasts.
Welcome back the show. This week, topic is a little more serious than usual. It is a story of surviving, an attempt at suicide.
So a couple of housecleaning things to note, because of the nature of our content is if in case you got a couple of kiddos sitting in the back seat, maybe skip this episode or maybe wait until you can throw on the headphones.
Also to note, we, Maggie and myself are not licensed mental health practitioners. Please, please. if you are in crisis or seeking help, reach out to your local crisis center or suicide hotline, and note on editing, due to the gravity of this conversation, I, myself was very nervous. Maggie was very courageous; there are some long pauses in between the question and the answer and those have not been heavily edited out.
My hope is that you can feel the gravity of, of the room as we were, trying to share this story as Maggie was trying to share her story. So with that, I’m going to jump right into it. I really hope this adds value and we’ll talk to you soon.
……….
We’re podcasting. Isn’t this fun?
Maggie Fage: [00:01:26] Oh my goodness. I’m so nervous.
Steven: [00:01:29] Yeah. That’s okay. I am too.
Maggie Fage: [00:01:31] Yeah. Yeah.
Steven: [00:01:33] But I mean, that’s a, I don’t know, but in all seriousness, we’re here to talk about mental health and we’ve had some family experience with it. It’s it’s run through our family. We have dealt with our own challenges growing up and now in our adult lives, maybe some of our childhood has affected what we’re dealing with now in our adult lives, but we are going to get right to it.
So today we’re here to talk about something that happened three years ago.
Maggie Fage: [00:02:06] Yes.
Steven: [00:02:06] Three years ago. What, what month, may? Okay. So it’s a very serious topic for anyone who’s listening. So Maggie, thank you for being on the show and for having courage to do this.
Maggie Fage: [00:02:19] Thank you for having me.
Steven: [00:02:20] It doesn’t go without saying…
So today we’re talking about suicide and suicidal thoughts and everything to do with that. So, we’ve got a story to tell and to share with all of you, because it’s, it’s, becoming a big issue. It’s a big issue in families. It’s a big issue in business. It’s a big issue in different cultures from man to woman it’s it’s becoming a big deal.
And I wonder if it’s worse than it’s ever been, or for just now more aware of it, with Robin Williams and Kate spade and all those happy faces. So there there’s a lot to talk about here, so
Maggie Fage: [00:03:00] They were hurting the whole time.
Steven: [00:03:01] All the time. So to set context for this episode, Maggie, will you share with us what happened three years ago in May?
Maggie Fage: [00:03:12] Um, so…
Three years ago, I hit a breaking point. I hadn’t really been doing good the past few years before then.. This probably all just led up to; honestly, I just hit, I hit the end.
I didn’t want to be here anymore and before I always made excuses of why to be around and yeah. At that point, three years ago or so I wasn’t making excuses anymore. I didn’t have any, anything. I knew my son would be okay because his father is around and he was moving in with him anyway. So.
Steven: [00:04:30] So when you, you visit, you ran out of, ways to justify or were you tired of the same justification?
Maggie Fage: [00:04:39] I think I ran out of justifications and the one that I always had always, always number one was my son. Like I said he was going to move with his father anyway. So I was like, okay, you’ll be fine. And, that was it.
Steven: [00:04:56] So what led up to that point where you officially ran out?
Maggie Fage: [00:05:04] I honestly don’t know. It was a long tiring journey. I had gone through a divorce, moved out. You know, with my son, it’s just tiring. It was just really tiring.
I gave up, I gave up.
Steven: [00:05:30] So for anyone that’s listening might be wondering you and I both know, are you comfortable sharing what giving up means?
Maggie Fage: [00:05:40] Oh, of what happened or so I’m, I was going to a provider who, quite frankly, I don’t believe should be practicing. I had a lot of extra psych pills laying around.
She would always like prescribe me something, like to try it out and it didn’t work, but she’d give me refills of it and in all honesty it was way too many pills that I, that I should have had. But anyway, so I had a lot of pills sitting around and I just, I, to be honest, I don’t know what I took, but I know I took a lot.
So I took a lot of pills. I think I had some sangria. I’m told there was, a note. I don’t remember writing that. And, I was actually, attached to my bedroom door knob. I was hanging there, something around my neck, hanging from the doorknob.
Okay. And then I woke up in the ICU.
Steven: [00:06:51] Do you remember how you felt when you woke up?
Maggie Fage: [00:06:58] I don’t remember initially, but I was told that I was in a rage and they actually had to tie me down. They called it a suicidal rage. Okay. I was pissed off because I was still alive.
And again, I don’t remember that part from what I do remember. I was like, Oh, hi, you guys like, Oh, thanks for visiting. Like, I wasn’t like thinking that I just did what I did, where everybody’s looking at me, like all exhausted. And like, you’ve been in the ICU for seven days and we didn’t know if you were going to wake up.
And I woke up, I was like, dootoodoo, like, I had no voice. There was a struggle getting the, the, the pipe down my throat. They, I’m trying to think what it’s called.
Steven: [00:07:53] Was it a breathing tube?
Maggie Fage: [00:07:54] Yes. Okay. There was a struggle with that. Um,
So yeah, I, I don’t have much memory of what happened.
Steven: [00:08:06] Do you remember? So when you woke up, you mentioned dootoodoo kind of thing, you know, just like kind of here. Did, did you get to a point where you were like, Oh shit? When you kind of realized how you had gotten here once, because I imagine you were on some medication while you were in the bed, like kind of sedated a little bit.
Maggie Fage: [00:08:26] Yeah, right…
Steven: [00:08:26] So did you come to, to a certain point and go, Oh shit. That’s how I got here.
Maggie Fage: [00:08:31] Not until I got to the psych hospital when I was in the regular hospital. I didn’t, I didn’t feel like you’re stupid shit. Do you know what you really did? I didn’t realize anything really until I get to the psych hospital.
Steven: [00:08:44] Hmm. And how did that feel?
Maggie Fage: [00:08:46] Horrible. That was horrible. It’s like really I’m in a psychological hospital and I have to be here. I was committed there. I didn’t have a choice. Yeah.
That’s when it hit what I had done, but I was still very angry. Because when the doctors tried to talk to me, I didn’t want to hear nothing. I just wanted to go home. but nobody would let me go home.
Steven: [00:09:23] What was the anger about?
Maggie Fage: [00:09:26] That I was there, that, you know, people were arguing with me. The doctors were like, You need to do this, this, this, and this, and you need to take this and you’re going to do this and you “yo!”, like I just met you like, and..
Steven: [00:09:46] So feeling like you didn’t have any control?
Maggie Fage: [00:09:48] Yeah. Hmm. Hmm.
Steven: [00:09:52] So then what happened next? Once you were released?
Maggie Fage: [00:09:54] So I was in a psych hospital for a month. And at the end of my time, probably like the last week I was there, we had decided to try what’s called ECT, which is electrical something shock. I’m sorry, I don’t, I don’t know what the exact, but it’s electrical shocks and I agreed to try it.
Because rarely, no medicine I felt was helping me. And to be honest, the ECT saved me. It really did help me when I first did it three years ago.
Steven: [00:10:32] Can I jump in real quick? Yeah. So ECT, when you say electric shock, they put pads on your, on your head?
Maggie Fage: [00:10:38] Yes.
Steven: [00:10:39] And very specific spots.
Maggie Fage: [00:10:41] Okay. And they set it to certain measurements and it sends a shock through your brain.
Steven: [00:10:48] To kind of reset?
Maggie Fage: [00:10:49] Yes.
Steven: [00:10:50] Okay. Okay.
Maggie Fage: [00:10:52] Yes.
Steven: [00:10:52] So that worked?
Maggie Fage: [00:10:54] That worked tremendously. It’s worked better than any meds I’ve ever been on. And I’ve been on medicine over 20 years now.
Steven: [00:11:05] So when you say it worked, can you describe in any way possible the difference? Let’s say April the month prior to May when it happened. Okay. And then when you actually felt like, Oh shit, this kind of works.
Maggie Fage: [00:11:22] So I didn’t feel as heavy, like before I felt very weighed down; very dark, very, very, I don’t want to be here. And afterwards I felt lighter. I felt okay, the Frick, I can do this. What the hell were you thinking? Like you have your precious little boy, like you have, you have all these things. You need to be here, you know, and it gave me that little oomph to, to move forward, to do what I was, should be doing to help myself, whether I get my butt to counseling, whether it be, find a different job that’s not as stressful, whether it be… just actually motivation because I could just sit on the couch for 24, seven and disappear.
Steven: [00:12:19] So I’m really curious. What is that magic spark? You know, if, if you get to the point where you feel like I can do this, I have what I have. I have what I need to take care of myself.
What is it that caused you not to see those very same things that were present. In April the month prior. So there’s something inside that kinda that’s, that’s what I’m trying to figure out. You know…
Maggie Fage: [00:12:45] I think it’s definitely a big chemical imbalance that I have. And just by that point, it was years and years and years of it, you know, I was technically diagnosed with depression and anxiety in high school.
But I personally think I had it before then. So it’s just been a lot of years of just constant doubting yourself, really.
Steven: [00:13:15] So when something like that happens, I call it it’s like paper cuts. So maybe it’s not something extreme, but it’s years and years and years. And it sounds like how you described it. Towards what might’ve been the end. It was, was it just pure exhaustion?
Maggie Fage: [00:13:32] I believe so.
Steven: [00:13:33] Exhaustion of the spirit of like of just everything.
Maggie Fage: [00:13:37] No spirit, I had no spirit.
Steven: [00:13:38] Everything. Yeah. Wow.
Maggie Fage: [00:13:41] I had nothing. I had nothing left in me.
Steven: [00:13:47] Hm.
Maggie Fage: [00:13:51] Yep. And nothing.
Steven: [00:13:53] So that was three years ago. And you and I spoke on the phone a couple months ago and we was coming up on the reunion. And I remember you were saying you were feeling kind of funny. And my question was, is it possible that you could be feeling funny because it’s the reunion. And, or not to negate, but, and, or you could just be feeling funny, but now that we look back, we realize it had been some time since that you see ECT treatment.
Is it kinda more, that was two years ago, right? That you had your last one? Correct? Was that more of a subtle thing, but it was month after month after month, just kind of chipping away. Or how, how did, how did it kind of come back, do you think?
Maggie Fage: [00:14:46] Um, okay. So I think when we had the phone call, I think I told you that I didn’t think it was because the anniversary of it was coming up.
But I mean, logically of course, I’m sure it was. Yeah. But as far as the ECT, treatments, I continued them after I got out of the psych hospital, I was doing them about once a month after I had the initial six, treatments, I was doing them down in Florida and ended up moving down to Florida with my Dad.
And he helped me find doctors and all that down there. And I was getting them about once a month. Okay. And then I moved back up to Rhode Island and. I didn’t feel like I needed them anymore. I felt like I was okay. I didn’t need any more act, but I think that was a mistake because like you said, I hadn’t had a treatment in about two years and I think it was building up again, you know, not as bad.
As before, but I think I definitely should have stayed maintaining the ECT treatments, getting them about once a month, once every couple of months, something like that. And I really do think this wouldn’t have happened this, this, about a month ago or so I just wasn’t feeling right. Yeah. So I made a phone call.
I called my mom. I said, mom, I’m not feeling right. And that’s really all I had to say. And she came over and got me. I ended up going to the psych hospital again, I go to a psych evaluation, and I ended up staying there for about a month. The difference in this time from last time is that I did not harm myself.
I did not take pills I wasn’t supposed to, I did not drink to go, go back a little bit. I, I was a cutter, I say was because I have not cut in three years. And, I was a cutter from a very young age. Probably around 12 or 13. So I did not cut myself. I did not take any pills. I, I just knew I didn’t feel right.
And I knew I needed help and I knew I needed to get another ECT treatment. So that’s exactly what I did. I went to the hospital and they started me on the ECT. I’m currently still doing the ECT treatments more far more frequently than I’d like to be. But it, it will, it’ll level out soon. I’ll get down to like once a month, once every two months or something.
But I know now I need to maintain that because that really does help me because I have found that the medication alone doesn’t isn’t enough for me.
Steven: [00:17:44] So for anyone that’s listening, when you say started not to feel right. So that could mean very different things for very different people. And there are a lot of people may be listening who have loved ones who may be going through similar circumstances.
It’s hard to see on the outside, maybe for some people it’s hard to see on the inside. So what for you means “start to feel different?”
Maggie Fage: [00:18:13] So I started having thoughts of, “I don’t care.”
I don’t care. I’m not doing anymore. I’m not doing, I’m not going to work. I wasn’t going to work. I kept calling out of work, which is a big sign and I knew something was going on. I just knew sometimes you can’t pinpoint it. And I just knew that I was changing and I did not want to get deeper into that
Steven: [00:18:43] Hmm, so what is… oh man. That’s so it’s almost that you had been there before?
Maggie Fage: [00:18:55] Yes. I felt, I felt it coming and I was like, Oh no, no, no, you’re not coming back, but I don’t feel good. So I need to do something now.
Steven: [00:19:06] So the blessing there is the fact that you didn’t want to fall in. You still had the fuck it, you still had the, I don’t care, but there was just that tiny little glimmer to say, “not again.”
Maggie Fage: [00:19:17] Yes. Yup.
Steven: [00:19:20] Cause that’s all it takes, right?
Maggie Fage: [00:19:22] Yes. I mean, I could have easily gone and did what I used to do. Sliced something, take an extra pills, but I didn’t do any of that. I said no.
Steven: [00:19:39] So you have your you’ve taken your you’ve. You’ve had your ECT treatments. How many of those did you recently have?
Maggie Fage: [00:19:48] I’ve had several, I’ve had, I want to say I’m up to about 10 right now. It’s been a little over a month. They start you off frequently, like every other day. Monday Wednesday, Friday. And then after a couple of weeks of that, you go to once a week and then right now I’m on every other week.
Steven: [00:20:09] And are you, do they do medication and ECT at the same time?
Maggie Fage: [00:20:13] So for me, yes. I’m still on my medication. I do both too. Yeah.
Steven: [00:20:19] And what happens, after your ECT treatment? You’re a little foggy?
Maggie Fage: [00:20:23] I am.
Steven: [00:20:23] Okay. What other side effects have you experienced?
Maggie Fage: [00:20:26] So I would say the main side effect is, some memory loss
Steven: [00:20:30] Permanent or…?
Maggie Fage: [00:20:33] Yes.
Steven: [00:20:34] Okay.
Maggie Fage: [00:20:36] Yes. Easily forget things easily. You know, I’ve had conversations with you and I don’t remember what we said. Totally oblivious to it. Like I’m like really? I’m so sorry. Like, but that that’s my biggest issue is the memory loss. You do feel groggy afterwards. You’re under anesthesia every time. So that’s something to consider, but to me, the anesthesia and the memory loss, I’m fine with, if it helps me continue on.
Steven: [00:21:13] Hmm. So if you could have, you said it started when you were 12?
Maggie Fage: [00:21:19] The cutting?
Steven: [00:21:20] Yes.
Maggie Fage: [00:21:21] It was around 11, 12. Yup.
Steven: [00:21:23] If you could, for whatever reason, go back and have a conversation with that little girl, knowing what you know now, having the spark that kept you this time, because you’ve been there before, what would you tell that 12 year old girl?
Maggie Fage: [00:21:39] Go talk to your mother.
So we had some unresolved issues that was painful to me.
Steven: [00:21:52] So maybe it’s unresolved emotional trauma that sits inside us and just festers. And it turns into all these other things, maybe seemingly unrelated, but it all comes back to those core issues that haven’t been dealt with, whether we’re children or adults.
Maggie Fage: [00:22:13] Yeah. So I’ve always said that physical pain is better than emotional pain is what I’ve always said.
Steven: [00:22:23] So is that,
Maggie Fage: [00:22:24] I can he handle it better?
Steven: [00:22:25] Is that what the, the cutting…
Maggie Fage: [00:22:28] That’s what the cutting does. Yup. Then you, you, you cut or I cut and you’re like, cool. I feel better. Like it gets the other thing that’s bothering you pushed back. It doesn’t, it doesn’t fix it. It just pushes it back. And that’s what keeps building up.
Steven: [00:22:50] Kind of like back in the day when you had a cut and one of the old timers would slap your knee and say, okay, does that cut still hurt?
Maggie Fage: [00:22:56] Right. Right.
Steven: [00:22:57] Exactly. Wow. So that’s thank you for sharing that. That’s your 12 old self now, what might you say to anyone who’s listening who is maybe you a year ago or four years ago? You know, what is something they can consider? When they’re feeling like they’re running out of gas?
Maggie Fage: [00:23:17] Well, I can say is try to find somebody that you trust to talk to because I fought a lot. I fought with the therapist. I fought with the idea of having to go to a therapist, counselor, things like that.
Cause I just didn’t want to talk about it. I didn’t want to talk about all these things like from when I was eight years old. Cause that’s really when things happened that really bothered me, but you need to find someone to talk to and society has the thing about, you know, psych conditions, psych meds, psych this like that.
But if you need a little medication to help you. Please, you know, do that, look into ECT. That’s also another thing with magnets that they can do with your brain look into things. and if you’re young, if you’re a child, I know it’s hard because you have to get your parents on board with that. So
Steven: [00:24:21] Hmm, what was it?
Thank you for sharing that. What created that resistance for, you say you want to, didn’t want to talk about air quotes, all these things. Why, why do you think there was that resistance to having those conversations, whether it was a family member or a psych therapist or, or otherwise?
Maggie Fage: [00:24:40] I really don’t know why I didn’t, why I was so resistant.
I guess, because I knew there’s nothing you can do about it. That happened, things happen, but I didn’t get the fact that you have to heal from it. You can’t just keep, keep going. You can’t. Well, I, well, I can’t keep going because this is what happens to me. Some people can, I guess.
Steven: [00:25:09] So for people who are struggling with emotional trauma and maybe the family member is not around to have that conversation. this is maybe an unanswerable question. I’m still searching myself. How do you find resolve and peace when maybe you can’t have that conversation
Maggie Fage: [00:25:29] With the person that, that the pain is maybe coming from?
So I did that for a lot of years, actually. So let me just tell you when I was eight, my parents sat me down and told me that I was adopted by my dad, who I thought was my dad, your dad. And that my biological father, you know, was never around and want me, blah, blah, blah. So I’ll I found this out when I was eight, but at the last words that I’ll always remember, and anyone can argue with me, but they are, the truth was I’m not going to help you find him because I don’t want to see him.
And so from then on I didn’t talk,I didn’t talk. And that bothered me for a long time. I actually only just met the man last year and I was 38 years old.
Steven: [00:26:32] That’s 30 years later.
Maggie Fage: [00:26:34] 30 years later.
Steven: [00:26:35] Wow. Yeah. That’s a long time to hold on to all that.
Maggie Fage: [00:26:41] Yeah.
Steven: [00:26:44] So were there years where you almost tricked yourself thinking “I’m cool with this.”
Maggie Fage: [00:26:49] Yes
Steven: [00:26:49] …and deal with it and then it will kind of creep up on you.
Maggie Fage: [00:26:52] Yes. And that’s what happens. It kind of just creeps up on you. Well, on me.
Steven: [00:26:59] Well, that’s the scary part. It’s it’s when we think we’re doing just fine, maybe we numbed ourself enough we distracted ourselves enough and then all of a sudden,
Maggie Fage: [00:27:10] Pow.
Steven: [00:27:12] Pow. So that’s kind of the internal side for anyone who’s listening and maybe not personally struggling with this, but maybe has a family member, from your point of view, experiencing how your family members have responded good, bad, otherwise indifferent.
How might a listener who is, has a family member who is struggling? How might they. How might they respond? How might they approach, how might they raise the question for someone that they’re concerned about? Because I think something that society is struggling with is obviously the stigma of mental health.
Then it’s do I bring it up or do I not bring it up because it’s cool or uncool, or I don’t want to insult them or belittle them, or they maybe just don’t know how might a family member approach someone. Obviously it’s different for everybody, but what are your thoughts on that? Because there are parents out there who are feeling helpless and they want to help how having trouble getting this question out.
Maggie Fage: [00:28:18] I understand what you’re trying to say. So, it’s very important not to judge the person and it’s very important not to say “snap out of it”. Just feel better. You have nothing you have nothing to be depressed about. Don’t say things like that because that’s what will shut the other person up and in and won’t communicate with anybody. I’ve heard that for years.
So just be real. Just go, you know, if, if you think somebody is having a hard time, just talk to them. So, you know, what’s the matter to, you know, us the matter. Is there anything I can do for you? Anything that would help do you need me to take you to the hospital?
You know, do, do we need to get your meds checked? Anything to help them? Don’t put anything on them. They’re already feeling bad enough and it’s, it’s really not your fault.
Steven: [00:29:24] Who’s fault to be clear?
Maggie Fage: [00:29:25] It’s not the person who’s going through depression and all that. It’s not it’s believe me, it’s not something that you want to have.
Steven: [00:29:35] Right
Maggie Fage: [00:29:35] You can’t just snap out of it.
Steven: [00:29:38] And if I may add, the counterintuitive thing to remember is people who push us away are the ones who need a hug. So if they push you away, try so hard not to take it personally and say, Oh, screw them, they’re being a jerk. They’re pushing me away. Leave them, let them go off and be a jerk. No, those are the ones that need a hug.
Maggie Fage: [00:29:59] Yeah. So I’ve been in situations where I’ve, I know people have needed help and I’m just very consistent, you know, what do we need to do? Where do we need to go? What can I do? You’re sleeping at my house tonight. I’m bringing you to the hospital and don’t give them a choice because a lot of times they can’t make the choice
Steven: [00:30:24] or they feel like a burden.
That whole thing. Oh, I don’t want to bother you. I don’t want to take up space. That whole thing.
Maggie Fage: [00:30:29] There’s one instance where I did, I took a girl right to the psych hospital. I said, come on, we’re going. Because of the things that she was telling me that she was going to take all her pills and she was going to do this and that, I said, all right, come on.
Do you need an evaluation and she didn’t fight me on it. You know, people that are timid or say they don’t know what to ask. That’s not good for people like that.
They need somebody who’s stable and who can do it, who can do it for them.
Steven: [00:31:08] So now that you you’ve learned quite a bit, You’ve gone through the ringer. You’re on the other side, which I’m very grateful for. What comes next?
Maggie Fage: [00:31:20] So I have to really just maintain, keep maintenance going. I, myself, am going to keep up with the ECT. I’m going to try to get it to about once a month or once every couple of months or something I’m out also in counseling.
And I take my medicine. The biggest thing for me is just keep an eye out for the signs of the signs of depression coming up, or signs of just feeling, not feeling right hopeless. I don’t know how to explain it really, but it’s, it’s more of, “I don’t care” when I start calling out at work or when I start, you know, not caring about a darn thing I know too. All right. Pay attention to something going on right now.
Steven: [00:32:14] So that’s, I’m going to push this a step further. So regular treatments, talk therapy, paying attention to the signs or the triggers. I feel that’s addressing the root cause. That’s getting you to a point where you can build a life to where it gives you the capacity to build a life, but then what comes next?
What, what else can you do to prevent that hopelessness? Is it structure? Is it habits? Is it a job you love? Is it hobbies? Is it, how do you build a castle on the foundation that you’ve already now created?
Maggie Fage: [00:32:54] I would say you just keep moving forward. So I try to just stay at a situations where I know I’m going to be uncomfortable or places make me too anxious. I just won’t go there or certain people, and maybe I don’t need to be around anymore. I just try to make the situation that I’m in better. Try to keep it at bay.
Steven: [00:33:19] Good vibes?
Maggie Fage: [00:33:19] Yeah. Good vibes. I don’t do anything. I don’t want to anymore where I used to all the time, do stuff I didn’t want to do. that wears on you. Um,
Steven: [00:33:36] Awesome…
So is there anything, you would like to share with the audience before we close out, something to consider, to think about, be it on the supporter side, or be it on the individual who may be struggling.
Maggie Fage: [00:33:51] Just to know if you’re struggling there, there are people out there for you. And if you can’t find somebody to talk to message my brother and he’ll message me and I can talk to you.
Steven: [00:34:09] Perfect. to sum that up, you are not alone.
Maggie Fage: [00:34:14] You are not alone.
Steven: [00:34:15] Love it. Thanks Mags. Love you
Maggie Fage: [00:34:18] Love you
Steven: [00:34:26] you’re not alone in neither is Maggie in her struggle. You know, it took a lot of courage for her to share this story with myself and all of you. So I want to acknowledge her for taking that huge step, both in personal healing and in doing her part in lifting the stigma. I hope this episode has given any one of you hope that you or your loved one can survive in one day.
Find the spark that keeps them fighting. Thank you so much for listening and supporting this episode. Talk to you real soon. Take care. .
Sign up to receive email updates
Enter your name and email address below and I’ll send you periodic updates about the podcast.
Connect with Guests & Host
Maggie Forte
Maggie Forte is a Live-In Caregiver at Home Care Assistance living in New Hampshire. She has been my sister for 36 years and I love her dearly. Maggie wants anyone who listens to her episode and wants to reach out, they can DM her on Instagram. The link is below her picture.